Clinical Decision Support System.
Purpose
The ideas and beliefs underpinning the discussions guide students through engaging dialogues as they achieve the desired learning outcomes/competencies associated with their course in a manner that empowers them to organize, integrate, apply and critically appraise their knowledge to their selected field of practice. The ebb and flow of a discussion is based upon the composition of student and faculty interaction in the quest for relevant scholarship.
Activity Learning Outcomes
Through this discussion, the student will demonstrate the ability to:
- Contribute level-appropriate knowledge and experience to the topic in a discussion environment that models professional and social interaction (CO4)
- Actively engage in the written ideas of others by carefully reading, researching, reflecting, and responding to the contributions of their peers and course faculty (CO5)
Requirements:
Post a written response in the discussion forum to EACH threaded discussion topic:
- This week we learned about the potential benefits and drawbacks to clinical decision support systems (CDSSs). Create a “Pros” versus “Cons” table with a column for “Pro” and a separate column for “Con”. Include at least 3 items for each column. Next to each item, provide a brief rationale as to why you included it on the respective list.
- The primary goal of a CDSS is to leverage data and the scientific evidence to help guide appropriate decision making. CDSSs directly assist the clinician in making decisions about specific patients. For this discussion thread post, you are to assume your future role as an APN and create a clinical patient and scenario to illustrate an exemplary depiction of how a CDSS might influence your decision. This post is an opportunity for you to be innovative, so have fun!
Adhere to the following guidelines regarding quality for the threaded discussions in Canvas:
- Application of Course Knowledge: Demonstrate the ability to analyze, synthesize, and/or apply principles and concepts learned in the course lesson and outside readings.
- Scholarliness and Scholarly Sources: Demonstrates achievement of scholarly inquiry for professional and academic decisions using valid, relevant, and reliable outside scholarly source to contribute to the discussion thread.
- Writing Mechanics: Grammar, spelling, syntax, and punctuation are accurate. In-text and reference citations should be formatted using correct APA guidelines.
- Direct Quotes: Good writing calls for the limited use of direct quotes. Direct quotes in discussions are to be limited to one short quotation (not to exceed 15 words). The quote must add substantively to the discussion. Points will be deducted under the grammar, syntax, APA category.
This is topic for this week I will get at least two scholarly reference for each threaded discussion. Thanks so much.
Clinical Decision Support (CDS)
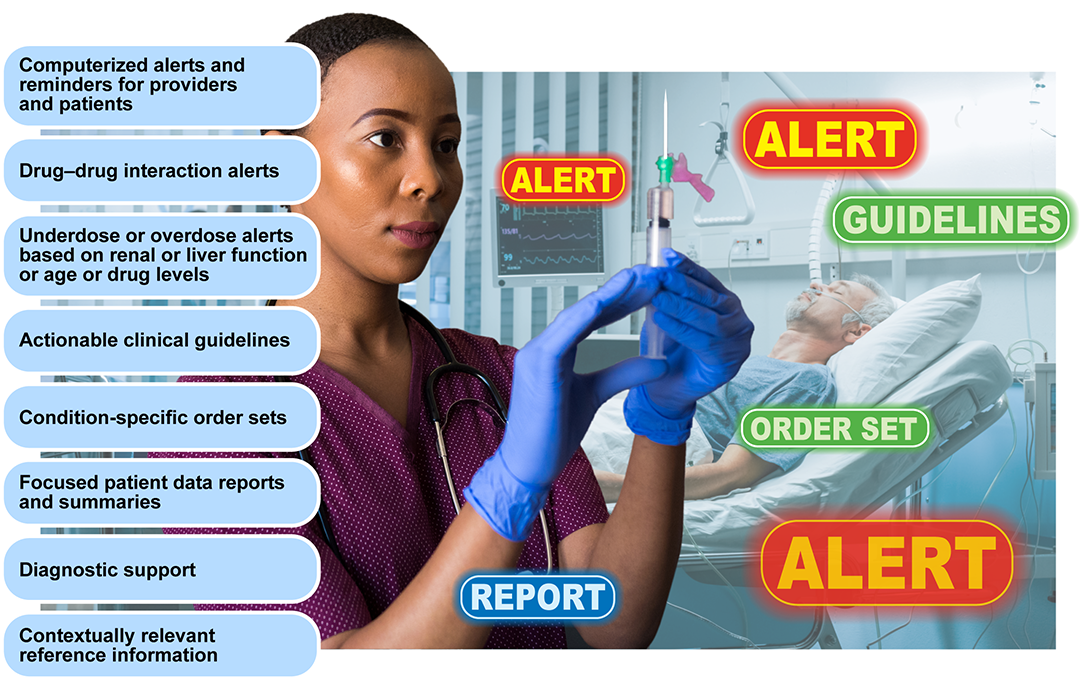
Clinical decision support (CDS) as a process designed to aid directly in clinical decision making, in which characteristics of individual patients are used to generate patient specific interventions, assessments, recommendations, or other forms of guidance that are then presented to a decision-making recipient or recipients that can include clinicians, patients, and others involved in care delivery. CDS tools existed prior to development of EHRs. Historical examples include practice guidelines carried in clinicians’ pockets, patient cards used by providers to track a patient’s treatments, and tables of important medical knowledge. The primary goal of implementing a CDS tool is to leverage data and the scientific evidence to help guide appropriate decision making. CDS tools include but are not limited to:
Workflow Design
Workflow is a term used to describe the action or execution of a series of tasks in a prescribed sequence. Another definition of workflow is a progression of steps (tasks, events, interactions) that constitute a work process, involve two or more persons, and create or add value to the organization’s activities. In a sequential workflow, each step depends on the occurrence of the previous step; in a parallel workflow, two or more steps can occur concurrently. The term workflow is sometimes used interchangeably with process or process flows, particularly in the context of implementations. Observation and documentation of workflow to better understand what is happening in the current environment and how it can be altered is referred to as process or workflow analysis. A critical aspect of the informatics role is workflow design. Nursing informatics is uniquely positioned to engage in the analysis and redesign of processes and tasks surrounding the use of technology.
Clinical Decision Support Systems and Improving Healthcare Delivery
Clinical decision support systems (CDSSs) are quickly becoming essential tools for healthcare providers as the volume of available data increases alongside their responsibility to deliver value-based care (Castaneda et al., 2015). Reducing clinical variation and duplicative testing, ensuring patient safety, and avoiding complications that may result in expensive hospital readmissions are top priorities for providers in the modern regulatory and reimbursement environment – and harnessing the hidden insights of big data is essential for achieving these goals. CDSS tools are designed to help sift through enormous amounts of digital data to suggest next steps for treatments, alert providers to available information they may not have seen, or catch potential problems, such as dangerous medication interactions.

Integrating CDSS into electronic health records allows medication information to be combined with patient information to create alerts about drug-drug interactions, drug allergy contraindications, and other important situations Drug-drug interaction checking and drug-allergy checking are conceptually straightforward but can catch a critical source of human error that no amount of training or personal vigilance can eliminate. A CDSs is not simply an alert, notification, or explicit care suggestion.
Slightly more advanced CDSSs analyze clinical data and present guidance based on those data. More sophisticated systems look for trends in values, such as the rate of fall of the hematocrit or the rising weight of an ICU patient who is accumulating extracellular fluid, where an absolute number may not be notable, but an alert to the trend may be important and prompt action. Such sophisticated tools require oversight by federal regulation, which we will address in more detail in the Week 6 lesson.
Challenges to Implementing a CDSS
Decision support systems are challenging to implement and maintain. The most vexing problem is “alert fatigue’. Studies within and outside health care show the benefit of an alert, such as a pop-up interaction in a software system, is rapidly extinguished if the alert becomes a routine part of using the system. In practice, 49% to 96% of alerts are overridden, raising questions about the effectiveness of decision support (Ancker et al., 2017). Alert fatigue and clinical burnout are common byproducts of poorly implemented clinical decision support features that overwhelm users with unimportant information or frustrating workflow freezes that require extra clicks to circumvent. One study found that clinicians spend approximately 66.8 minutes per day processing notifications from EHR use. Fant and Adelman (2018) concluded alarm fatigue to be a significant burden for clinicians. Alert fatigue is a fact of human cognition and cannot be eliminated through training, education, or vigilance. The best clinical systems offer fine-grained tuning of the system’s behavior, such as altering the system’s response by drug and provider specialty and offer a range of interruptive and non-interruptive support mechanisms.
The financial implications to design and maintain informatics infrastructure is often costly for any institution. The most complex decision support systems attempt to aid clinical diagnosis. The application of artificial intelligence to medicine has a long history; however, most diagnostic expert systems have been stand-alone, requiring effort by the clinician outside of their normal workflow and have thus seen limited clinical implementation. Examples of clinical diagnostic systems directly imbedded in an electronic health record are few but are an area of increasing commercial interest.
Why Incorporate a CDSS with Practice?
The primary goal of a CDSS is to leverage data and the scientific evidence to help guide appropriate decision making. When looking at ways in which CDSS tools can be leveraged in a clinical process, the CDSS team needs to approach the project from a data-driven manner supported by the evidence. This requires in-depth analysis of the scientific evidence coupled with data-analysis methods to identify gaps in practice within the organization. It is equally important to identify where there are gaps in ability to report how an organization is doing with respect to patient care and if recommended practice guidelines are being followed. This would constitute absence of data captured to track that information. Often, these gaps or absence of data and information tell an organization where to focus with respect to adding where a CDSS tool should be. It is the role of the CDSS team to identify all the elements of a process and use data to identify areas where processes might be enhanced with the use of CDSS tools to provide users with the best evidence and to support appropriate decision making and treatment decisions (HIMSS, 2014
this course is Nursing Informatics for Advanced Practice.
Answer preview
|